Have thyroid disease?
Congratulations, in addition to having to deal with one of the most difficult hormone problems to master you also have to deal with an increased risk of developing certain gut problems.
The good news is that knowing is more than half of the battle.
The reason for this increased risk has to do with something called the gut-thyroid connection (1).
In other words, the dynamic relationship between gut function and its impact on your thyroid and thyroid function and its impact on your gut.
This relationship is bidirectional.
The gut helps your body to activate and utilize thyroid hormone more effectively while the thyroid helps your gut to stay healthy by encouraging peristalsis and digestion.
If there is a problem in one system it will drag down the function of the other.
And that’s exactly why this topic is so important.
Today you will learn:
- More about how the thyroid impacts gut function and how the gut impacts thyroid function.
- Specific diseases that are more likely to occur when your thyroid is sluggish or decreased.
- Gut infections and their relationship with thyroid autoimmunity.
- Why thyroid patients are more likely to develop nutrient deficiencies and how these nutrient deficiencies impact thyroid function.
- And much more…
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Gut Issues Commonly Caused or Associated with Thyroid Disease:
Because of how the thyroid impacts your gut function, you are much more likely to develop certain conditions as a result of your thyroid problem.
Here’s why:
Thyroid hormone impacts a very important function of the gut known as peristalsis (2).
Peristalsis is a fancy word used to describe the constant rhythmic motion that your intestines undergo constantly.
This motion is responsible for slowly moving the contents of your gut (food, bile, acid, etc.) through your intestinal tract.
Peristalsis is not something under conscious control like other muscles in your body.
If you want to flex your bicep, for instance, all you need to do is think about it and move your arm and forearm close together.
The bicep muscle is under conscious control.
The same is not true for your gut!
You can’t consciously control how quickly intestinal contents are moving through your gut just by thinking about it.
Instead, other systems in your body, the autonomic nervous system as well as your thyroid, control it (3).
The more thyroid hormone stimulation you have on the gut the quicker your bowels will move.
This effect extends all the way to diarrhea as may occur in hyperthyroidism (4).
The less thyroid stimulation you have on the gut the slower your bowels will move.
This effect extends all the way to severe constipation as may occur in hypothyroidism (or low thyroid function).
And it is this slowing of your gut that sets the stage for the development of MANY of the diseases we are about to discuss.
It turns out that the speed at which your gut moves is very important…
#1. SIBO (Small Intestinal Bacterial Overgrowth)
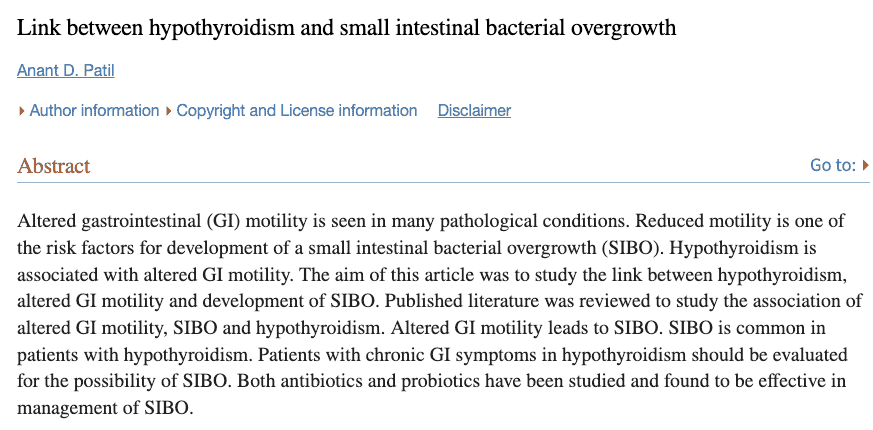
#1 and #2 which we are about to discuss often come as a pair and they are referred to as overgrowth syndromes.
Small intestinal bacterial overgrowth, referred to as SIBO, is a common gut problem among thyroid patients.
Some studies estimate (5) that as many as 50% of low thyroid patients suffer from this condition.
But what is it?
As the name suggests, it’s caused by an overgrowth of good (or bad) bacteria in the small intestines.
This occurs during hypothyroidism because of the transit problem I mentioned above.
As intestinal contents sit in your gut longer they are broken down and interact with bacteria longer than normal.
This provides a food source for the bacteria which allows them to grow in population.
As this occurs, they impact gut function, bowel movements, gas production, and many other issues.
It’s important to understand, though, if you have SIBO as a thyroid patient that fixing the gut motility problem should be priority #1.
You can kill off the overgrown bacteria with the use of herbal antibiotics or prescription antibiotics but if you don’t fix the motility problem then the problem will just recur.
#2. SIFO (Small Intestinal Fungal Overgrowth)
You can think of SIFO as a sister condition to SIBO.
Small intestinal fungal overgrowth, or SIFO (6) for short, is very similar to SIBO except the overgrowth in SIFO is from fungus.
The term SIFO is relatively new so you may be more familiar with the term candida which is often used to describe this condition.
The reason it’s commonly referred to as candida is that candida is responsible for the overgrowth in more than 90% of cases (7).
SIFO and SIBO both present with very similar symptoms but their treatments are a bit different.
The use of herbal antifungals or prescription antifungals can treat the overgrowth portion but, just like SIBO, you still need to address the motility problem.
SIFO may result in symptoms such as:
- Bloating
- Abdominal pain
- Gas production
- Diarrhea
- Nausea
- Cravings for sugary foods
These are largely the same symptoms as SIBO.
Because of the overlap you really want to make sure you test for both conditions at the same time.
If you are someone who knows you have SIBO, for instance, then it would be a good idea to also check for SIFO as well (or vice versa).
Forgetting to check for both conditions is one reason why some people remain symptomatic after treatment.
#3. Delayed Gastric Emptying (Gastroparesis)
Next up we have decreased kinetic bowel movements and gastroparesis.
Decreased kinetic bowel movements refer to a slowing down of the kinetics of your entire bowel and gastroparesis refers specifically to the stomach.
This is why gastroparesis is referred to as delayed gastric emptying (8).
While the thyroid does have some control over gastric motility it’s usually not strong enough to cause full-blown gastroparesis.
Instead, it typically causes a slowing down of gastric emptying which causes problems over the long term but usually isn’t sufficient to bring you to the doctor right away.
The symptoms associated with gastroparesis (or delayed gastric emptying) include:
- Heartburn or acid reflux
- Nausea after eating
- Vomiting
- Feeling full quickly
- Abdominal bloating
- And decreased appetite
These specific symptoms arise as your stomach is not able to empty quickly enough into the small intestines.
This is why people with gastroparesis often experience a lot of nausea after a meal.
There’s nowhere for the food to go so it refluxes back up into the esophagus (causing heartburn) and pushes against the wall of the stomach (causing decreased appetite).
Treatment of gastroparesis in thyroid patients should focus on improving the motility and movement of the stomach!
This means getting on the right type of thyroid medication (if necessary) to help move the contents of the stomach into the small intestines.
Some herbal options can also be used, such as Triphala (9), which can help boost gastric motility.
#4. GERD (Gastroesophageal Reflux Disease)
A very common gut problem among thyroid patients is acid reflux.
Even though many thyroid patients suffer from acid reflux (or GERD) it’s not as intuitive as you might think.
Here’s why:
As you will soon find out, decreased thyroid function often results in decreased stomach acid.
If that’s the case, why would thyroid disease result in acid reflux which is usually thought to be a problem with the overproduction of acid in the stomach?
Isn’t that a good thing?
Well, yes, and no.
And this is where things get a little tricky and where we aren’t sure exactly what is happening.

We know for sure that stomach acid is important for the breaking down of food, the absorption of nutrients, and for sustaining healthy populations of gut bacteria.
When stomach acid levels drop, you start to develop nutrient deficiencies, changes in bacterial concentrations in the gut, and problems with malabsorption.
It is felt that the inability to completely break down or process food in the stomach may be what is triggering acid reflux in thyroid patients.
As your body is unable to break down the food you eat, that food stays in your stomach longer and has more opportunities (10) to reflux back into your esophagus causing heartburn.
This theory hasn’t been proven scientifically but intuitively does seem to make sense.
What we know for sure, though, is that thyroid patients do experience acid reflux (11) even with low levels of stomach acid.
Whether that occurs via the mechanism listed above is somewhat irrelevant as the treatment is still the same:
Fix the thyroid and get off of acid blockers as quickly as possible.
Prolonged use of acid blockers is known to cause issues with thyroid function in many different ways.
If you are taking acid blockers daily (including things like proton pump inhibitors) then make sure to check out this article which will help you understand why it’s better for your thyroid if you can get off of them as soon as possible.
#5. Low Stomach Acid
Low stomach acid is another common gut problem that thyroid patients deal with.
The reason that patients with hypothyroidism can experience decreased stomach acid is that thyroid hormone plays a role in hydrochloric acid secretion (12) (AKA stomach acid).
As thyroid hormone levels drop so too does their impact on stomach acid.
As a result, stomach acid levels fall.
This low stomach acid triggers a host of different issues including acid reflux (as we discussed above) in addition to other problems.
One of those problems associated with low stomach acid is an increased risk of developing gut infections (13) such as:
- Clostridium difficile colitis (3x increased risk)
- Campylobacter
- Salmonella (2-6x increased risk)
- And SIBO/SIFO syndromes (2-8x increased risk)
That’s not all, though.
Decreased stomach acid also increases your risk of developing deficiencies in calcium, vitamin B12, Vitamin D, and magnesium.
All of which are important for overall health and thyroid health.
B12 helps to provide you with energy production via its impact on mitochondrial function.
Vitamin D can help fight off autoimmune diseases (like Hashimoto’s thyroiditis).
Magnesium is required for over 300+ different cellular processes.
And so on.
In short, you need optimal levels of these nutrients if you want to feel healthy and well.
You’ll often see thyroid patients, especially those with Hashimoto’s, recommend the use of supplements such as betaine HCl and pepsin for this reason.
These ingredients can help increase stomach acid levels naturally and fight off some of the issues that I just mentioned.
These supplements are great but you should still focus on improving thyroid function through the use of natural therapies or thyroid medication.
Increasing thyroid function will naturally increase stomach acid by virtue of its influence directly on the stomach.
#6. H. Pylori Infection
H. Pylori, short for helicobacter pylori, is a bacteria that can take up residence in the lining of your stomach.
It is most well-known as the primary cause of stomach ulcers among the general population.
It gets a lot more attention in the thyroid community, though, because it’s frequently associated with thyroid autoimmune disease.
In fact, studies have shown a link between H. pylori infections and both Hashimoto’s and Graves’ disease.
Some people believe that infection with H. pylori is enough all by itself to trigger Hashimoto’s and Graves’ disease and, therefore, treating it may provide a way to manage those diseases.
There is some evidence to support this idea including the idea that both the stomach and the thyroid gland share similar embryonic features (14) which may mean if one is susceptible to infection the other may be as well.
Other people dispute the idea that H. pylori infection is a primary cause of thyroid autoimmune disease.
As for me, I think it’s somewhere in the middle.
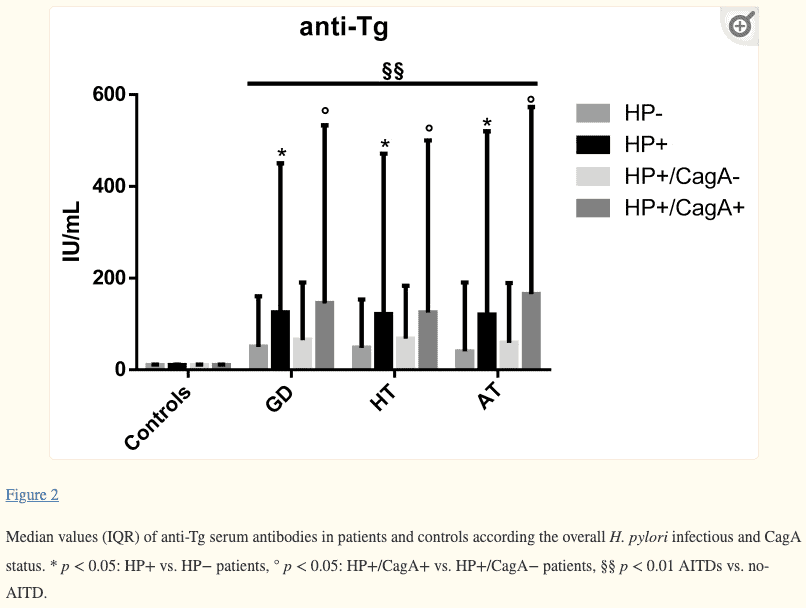
Regardless of where you sit on this debate, though, one thing is for certain:
If you have an H. pylori infection you need to treat it!
That’s really what’s most important.
If you treat and eliminate the infection and your thyroid improves, great!
If you treat and eliminate the infection and your thyroid does not improve, that’s still great!
Why?
Regardless of thyroid function, you never want to leave a smoldering infection sitting around in your gut.
Even if it doesn’t cause thyroid problems it will cause other issues that may directly or indirectly impact your thyroid down the road.
Unlike many of the other issues we’ve discussed so far, treating your thyroid with thyroid medication or natural therapies won’t make this problem go away.
You’ll most likely need medical care in the form of prescription medications or herbal/botanical supplements to eradicate the infection.
Prescription medications including things like antibiotics, Pepto Bismol, and acid blockers, may be necessary.
Some people do have success using herbal antibiotics, probiotics, and various other vitamins, so if you prefer the all-natural route you may be able to find some relief.
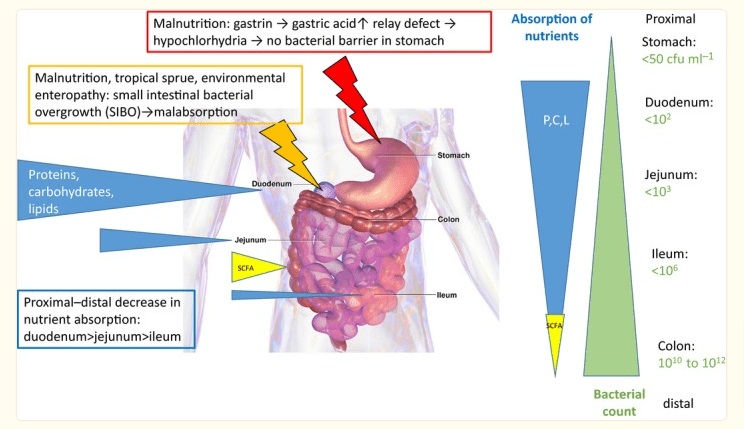
#7. Malabsorption
This one should make a lot of sense based on what we’ve discussed so far!
If your body can’t produce stomach acid then you will have problems breaking down and digesting your food.
And guess where the nutrients, vitamins, and minerals come from that your body uses on a daily basis?
The food you eat, of course.
If you are not able to digest your food appropriately then you put your body at risk of being incapable of extracting the nutrients it needs on a daily basis.
This is part of the reason that I’m always talking about the importance of replacing nutrient deficiencies in thyroid patients.
Thyroid patients, as a whole, are more likely to develop nutrient deficiencies compared to the general population.
Deficiencies in magnesium, vitamin D, zinc, selenium, iron, vitamin B12, and iodine are all very common among thyroid patients.
Many of these stem from issues with absorption (though not all) which is why taking thyroid support supplements is almost always a good idea.
True malabsorption syndromes are uncommon due to thyroid problems (15) but long-term suppressed thyroid function can certainly push you into the sub-optimal zones of many of the nutrients we’ve discussed so far.
And even if you don’t have a true deficiency, a sub-optimal level may impact your quality of life.
#8. Celiac Disease
Celiac disease and thyroid disease are one of those chicken and egg types of things.
It’s probably the case that untreated Celiac disease may trigger autoimmune thyroid disease (such as Hashimoto’s) but it’s also the case that those with Hashimoto’s are more likely to develop Celiac disease.
So which came first?
Did Celiac disease cause autoimmune thyroid disease or did the thyroid disease result in Celiac disease?
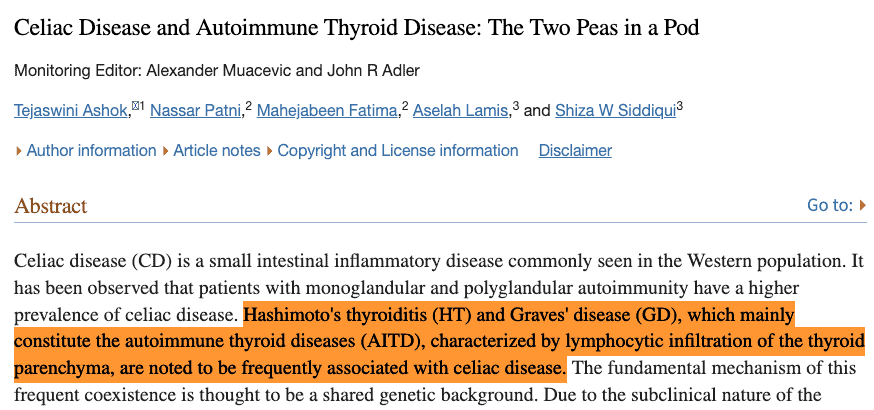
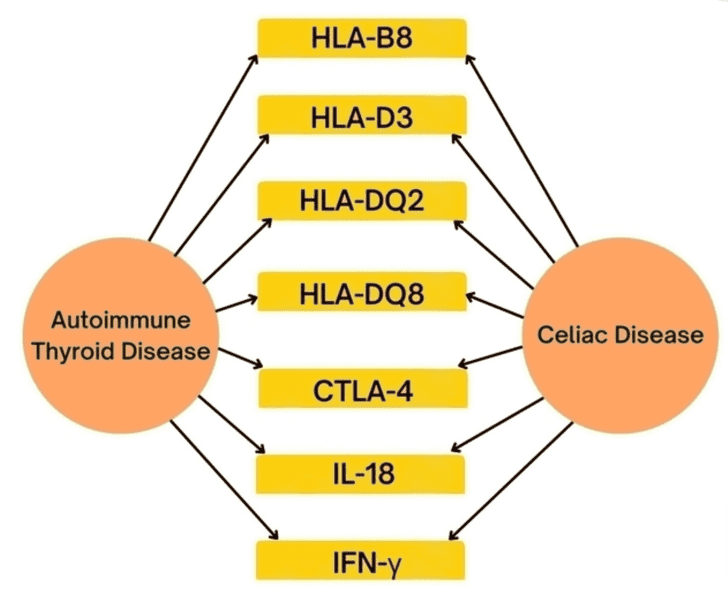
It probably depends on the person as each case is a little bit different.
What we know for sure is that gluten can cause problems for thyroid patients in two distinct ways:
- The first, Celiac disease (16)
- And the second, non-celiac gluten sensitivity (17)
Even if you are someone who doesn’t have true Celiac disease it still may be the case that gluten is not something you want to consume.
Those with something called gluten intolerance (NCGIS is the official name) still have problems when eating gluten, they just don’t develop the antibodies seen in Celiac disease.
My experience suggests that most thyroid patients do better when consuming little to no gluten.
This is a very controversial topic, though, as you might imagine and no one has the right answer as of yet.
But because the downsides to removing gluten from the diet are minimal to non-existent, it’s usually a good idea for thyroid patients to undergo a trial of removing gluten from their diet to see if they experience improvement.
#9. Gallstones
Gallstones are really coming from the liver but the liver and the gut are connected so I’ve included them here.
Thyroid patients are more likely (18) to develop gallstones for the following reasons:
- Decreased liver cholesterol metabolism – Decreased thyroid function slows down how efficiently the liver can metabolize cholesterol. This is one of the reasons why thyroid patients experience high cholesterol. And bile is one of the primary ways that the body eliminates cholesterol.
- Diminished bile duct secretion – Low thyroid function also slows down bile duct secretion which means that bile sits around longer which gives more opportunity for a gallstone to form.
- Reduced sphincter relaxation – Lastly, decreased thyroid function reduces how well the sphincter of Oddi works which means that it’s more difficult to move bile from the common bile duct into the intestines.
#10. Autoimmune Gastritis
Finally, we have autoimmune gastritis.
Autoimmune gastritis is another autoimmune disease which means that if you have autoimmune thyroid disease you are more likely to develop this condition as well.
Autoimmune gastritis results in the killing of specific cells in the stomach which produce stomach acid.
Thyroid patients with autoimmune gastritis may experience vitamin B12 deficiency and iron deficiency.
The reason for this has been explained in previous sections which outlined why it’s so important to have sufficient stomach acid in the gut.
Final Thoughts
Here’s the takeaway:
There is a strong connection between your gut and your thyroid gland.
As a result, thyroid patients are much more likely to develop certain gut-related problems compared to the general population.
Many of these problems can be prevented or treated by simply managing thyroid function.
This means getting on the right type and dose of thyroid medication or using natural therapies to boost how well your thyroid is operating.
Some gut conditions, though, can’t be treated or managed by just optimizing your thyroid.
These conditions may require the use of prescription medications or targeted natural botanicals or herbs to fix.
Now I want to hear from you:
Were you aware of the connection between your gut and your thyroid?
Are you currently suffering from any of the gut-related conditions discussed above?
If so, have you had success in treating or managing them?
Do you feel that fixing your thyroid is necessary to fix your gut?
Leave your questions or comments below!
Scientific References
#1. ncbi.nlm.nih.gov/pmc/articles/PMC7353203/
#2. ncbi.nlm.nih.gov/books/NBK556137/
#3. pubmed.ncbi.nlm.nih.gov/15788986/
#4. ncbi.nlm.nih.gov/pmc/articles/PMC2699000/
#5. ncbi.nlm.nih.gov/pmc/articles/PMC4056127/
#6. pubmed.ncbi.nlm.nih.gov/25786900/
#7. gastrojournal.org/article/S0016-5085(14)61294-4/pdf
#8. pubmed.ncbi.nlm.nih.gov/9356880/
#9. ncbi.nlm.nih.gov/pmc/articles/PMC5567597/
#10. pubmed.ncbi.nlm.nih.gov/8545632/
#11. ncbi.nlm.nih.gov/pmc/articles/PMC4087959/
#12. ncbi.nlm.nih.gov/books/NBK507793/
#13. ncbi.nlm.nih.gov/pmc/articles/PMC5615773/
#14. ncbi.nlm.nih.gov/pmc/articles/PMC7167994/
#15. pubmed.ncbi.nlm.nih.gov/1940412/
#16. ncbi.nlm.nih.gov/pmc/articles/PMC2111403/
#17. ncbi.nlm.nih.gov/pmc/articles/PMC6630947/
#18. ncbi.nlm.nih.gov/pmc/articles/PMC4940627/

Leave a Reply